The future of revenue cycle automation is here
70% automation of bill ready codes and claims with 95+ accuracy
PRACTICE.AI
The future of revenue cycle automation is here
70% automation of bill ready codes and claims with 95+ accuracy
Request Demo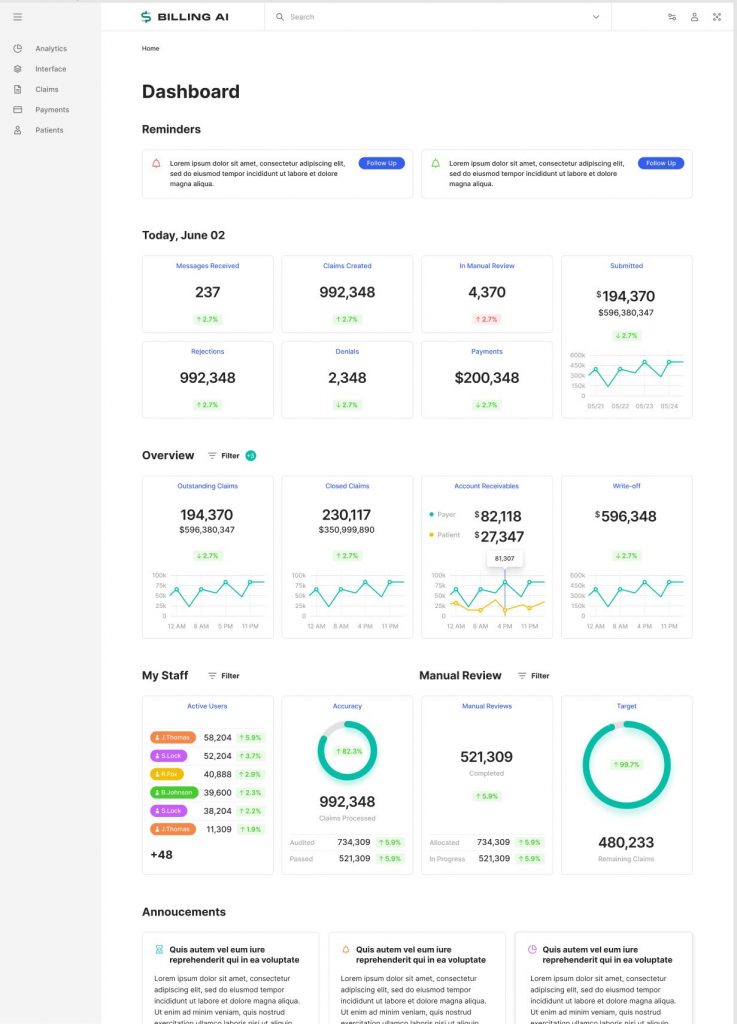
Outcomes
Automate claims submission, identify key trends, and improve your bottom line
Practice.AI automates end-to-end revenue cycle processes using NLP, Graphs, Logic based rules. The platform automates medical codes ( CPT, ICD 10, Modifiers, MIPS, G-Codes, Z-Codes ), bill ready charges, eligibility verifications, denial prediction and prevention, claim preparation, claim submission, claim reappeals, A/R workflow queue optimization, payer contract onboarding, payer contract analysis, underpayment analysis, EOB/ERA root cause analysis for line item wise denials.
Automate billing workflows
Manual processes plague the prevailing medical billing workflow, causing providers to leave significant dollars on the table. BILLING.AI automates the end-to-end medical billing process, including charge entry, eligibility verification, denial prediction and prevention, claim preparation, claim submission, adjudication, response, and A/R redirection.
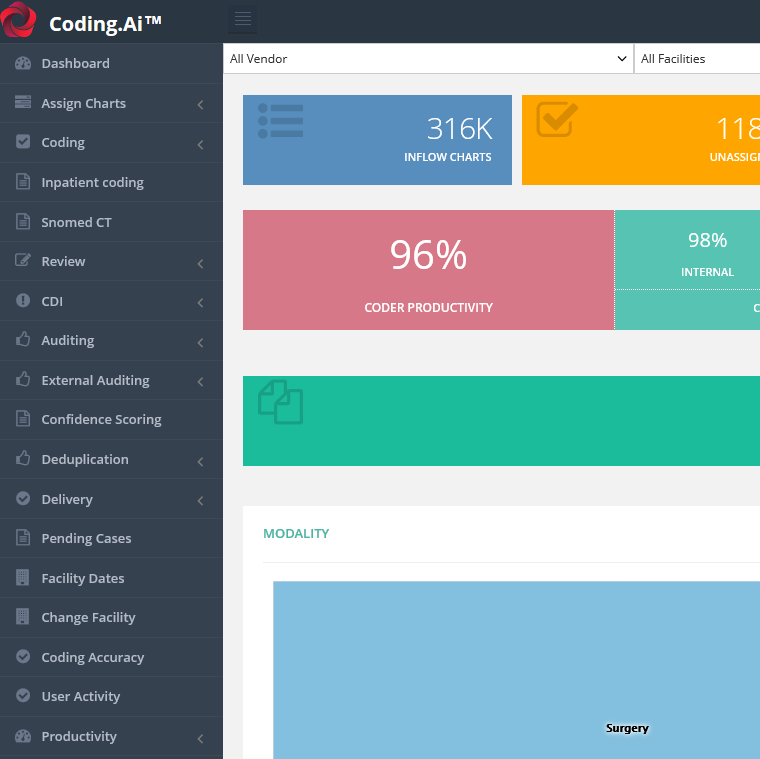
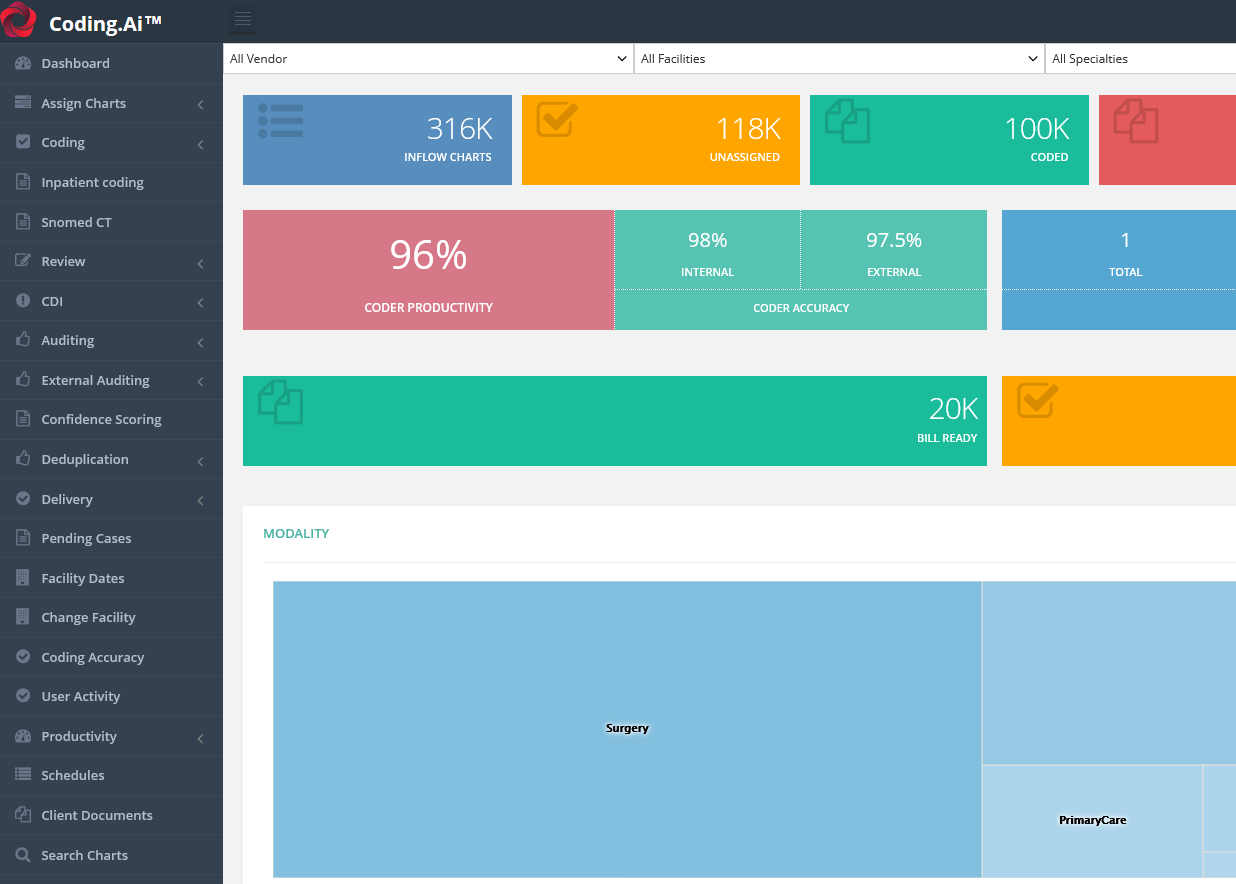
Reduce coding costs, guaranteed
Clients who have deployed CODING.AI report a minimum of 30% savings versus manual or computer-assisted-coding. By automating a minimum of 70% of medical coding volumes, CODING.AI helps you reduce denials and increase reimbursements without a massive investment in infrastructure and additional headcount.
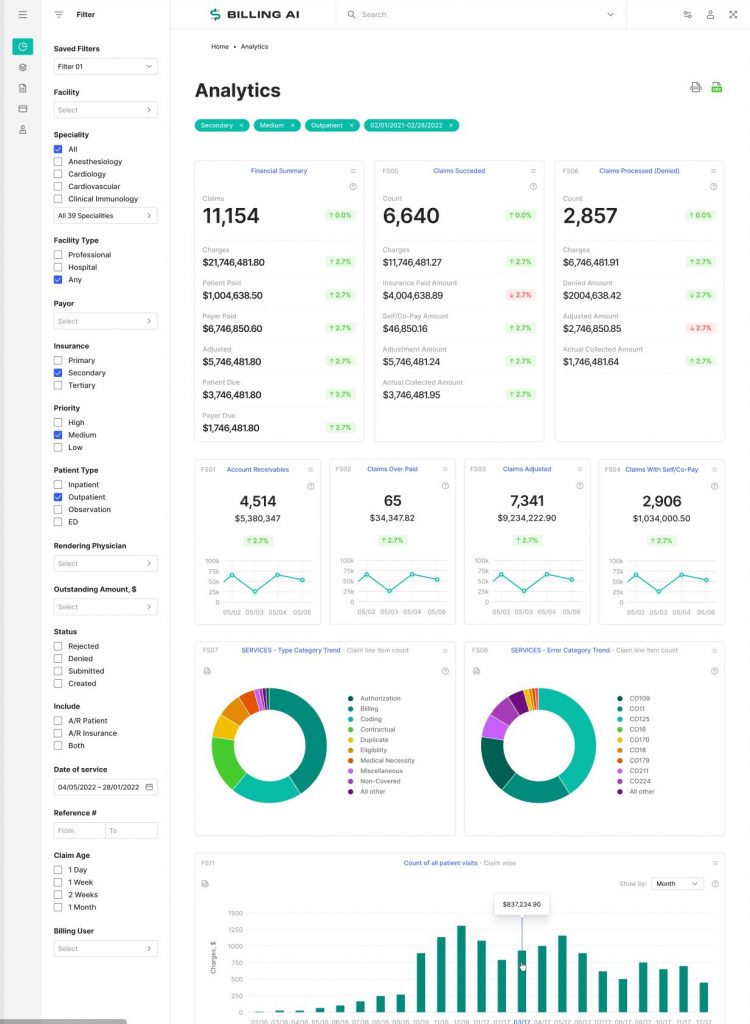
Identify key trends
Our best-in-class billing analytics module includes 140+ detailed reports that track an array of details salient to a provider’s financial operations. BILLING.AI automatically identifies and summarizes key trends so that you can take action.
Boost claims accuracy
Powered by industry-leading deep learning algorithms, CODING.AI is the most accurate medical coding automation platform on the market. We contractually guarantee 95% or greater coding accuracy.
Improve your bottom line
Prevent revenue leakage, reduce costly billing mistakes, and streamline the currently cumbersome claims submission process by automating your end-to-end billing workflow. Leverage BILLING.AI to reduce the lead time to get reimbursed for services rendered. BILLING.AI helps providers get paid more, quicker.
Ensure security and scalability
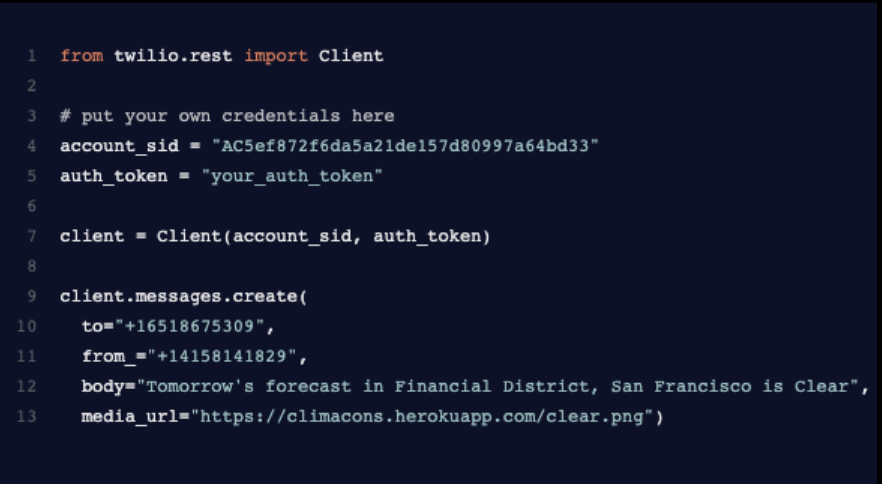
BUDDI.AI leverages Microsoft Azure to deliver best-in-class performance, security and scalability. We deploy CODING.AI within a fully HIPAA and SOC2 cloud and secure all patient health information and personally identifiable information through military-grade AES 256-bit encryption. It offers multiple hosting options to suit your needs.
PRACTICE.Ai
Features
- Smart Patient Registration: Simplifies the front-end patient intake process by capturing relevant information and documentation electronically with pre-reg options, including real-time insurance eligibility verification, to avoid delays and provide the best possible patient experience with mobile based appointments and payments.
- Prior Auth Identification: Applies natural language processing (NLP) and graph technology to autonomously identify certain clinical procedures which require prior authorization from the respective payer and kick starts the respective prior auth approval process, thereby cutting down significant labor time on a daily-basis and denials.
- Medical Coding Automation: Automates structured and unstructured coding volumes—often the most burdensome function of RCM—with 95% or greater coding accuracy contractually guaranteed, to help reduce denials and increase reimbursements.
- Denial Prediction & Prevention | Claims Automation: Analyzes historical denials, approvals, patterns or other payer behavior based on both BUDDI AI and the institution’s experience to proactively predict and prevent errors with claim submission, leading to reduced denials, faster A/R times and higher payer reimbursement. This real-time automation of the claims submissions process cuts down A/R times by 3X to 6X depending on the provider organization.
- AI Driven Denials Root Cause Analysis: Analyzes revenue leakage and reduces the lead time to get reimbursed for services rendered by eliminating the potential of manual error across the billing process, including explanation of benefits (EOB) root cause analysis. Based on RARC/CARC denial codes and automatically classified into respective denial work queues, an automated first-pass analysis is completed and then dropped into respective queues for experts, if needed, to conduct manual review prior to reappeal.
- Payer Contract Management & Under Payment Analysis: Onboards payer contracts and applies NLP and graph algorithms on the unstructured contract languages, mines the legal language—including pricing, expiries, sub-contract language, value-based care or Fee-For-Service contracts—and then creates a “Contextual Contract Graph” to analyze each incoming explanation of benefits (EOB) /electronic remittance advice (ERA) to identify under payments by respective payers and help reappeal those claims. Additionally, payer specific adjudication reports are generated in detail to re-negotiate contractual terms at the time of renewal.
- Web-based Patient Portal and BUDDI PAY app: Improves the patient journey and helps minimize drop-off by offering one-stop web- and app-based portals for patients to see and engage in their care continuum, from registration to bill payment. On an upcoming version, patients can take snapshots of their invoice and make payments for any provider bill across all 50 states in America. BUDDI Pay could dramatically improve patience experience by being the one-stop-payment app for patients around the country irrespective of the provider’s EMR or billing system.
Learn more about PRACTICE.AI
Schedule a demo today to see end-to-end practice automation in action.
Learn more