Automatically predict and
prevent claim denials
Outcomes
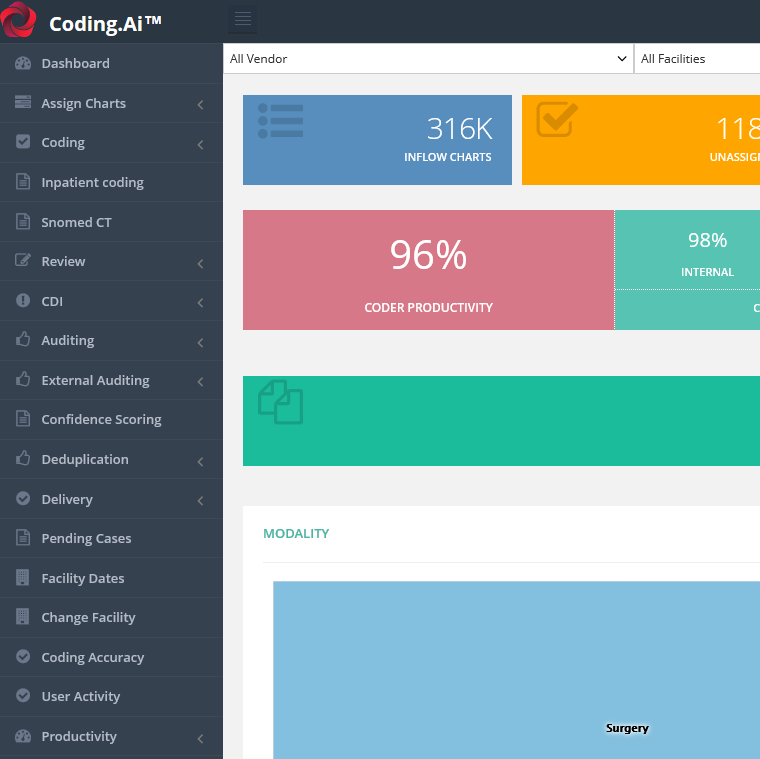
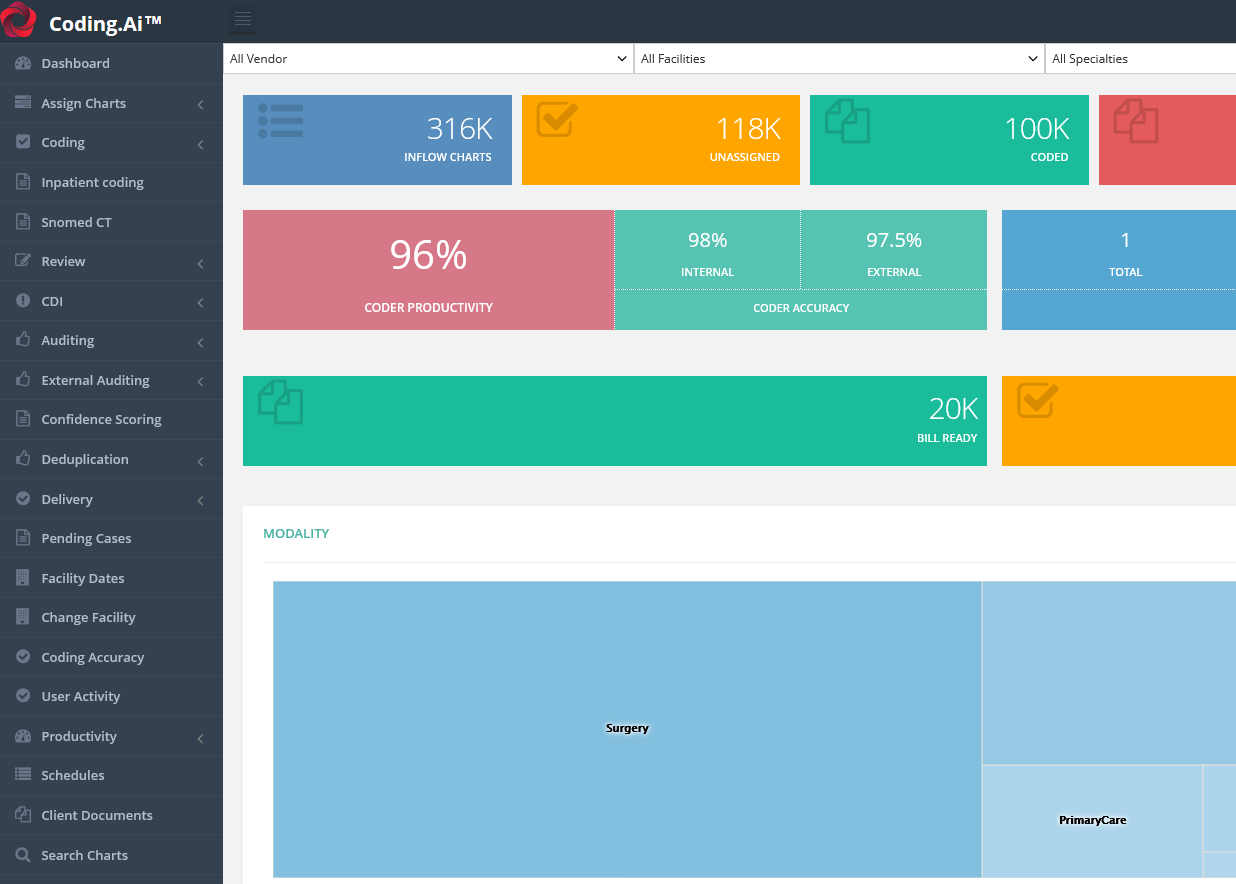
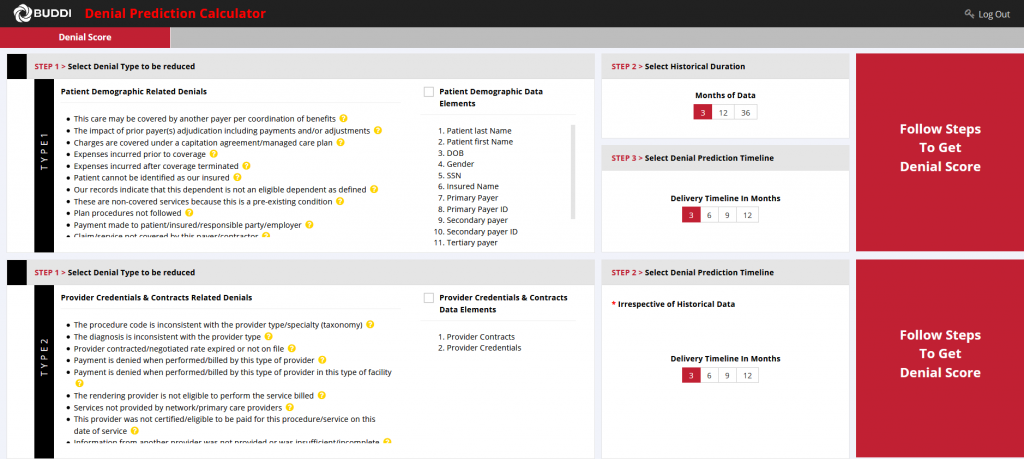
Claim denial prediction and prevention engine
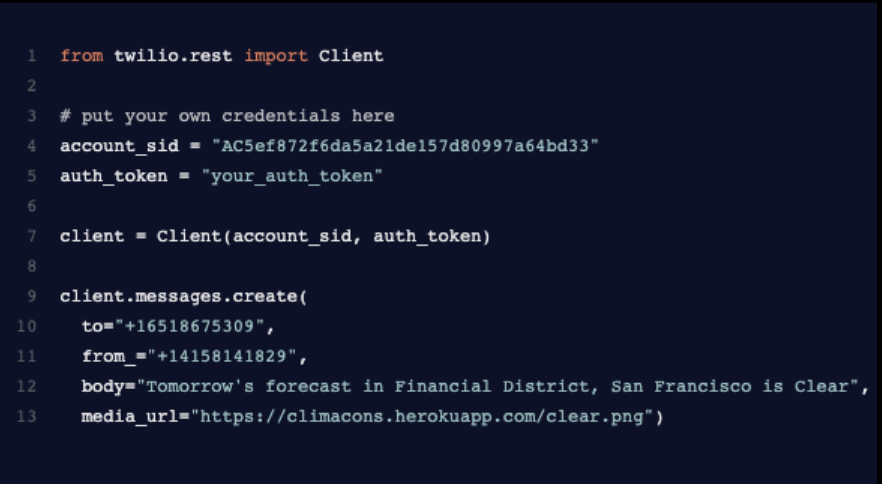
CLAIMS.AI leverages deep-learning to automate claims management, resulting in more accurate claims, significantly reduced denials, and higher payer reimbursements.
Improve claims accuracy
CLAIMS.AI analyzes historical denials and approvals, as well as EOBs, medical codes, CARC/RAC codes, payment patterns, and other payer behavior to proactively identify errors before claim submission, decreasing odds of denial.
Reduce claim denials
Clients who have deployed CLAIMS.AI report a 40% average reduction of denials within 12 months of launch.
Boost payer reimbursements
A typical health system stands to lose as much as 3.3% of net patient revenue (an average of $4.9M per hospital) due to denials, per a study by Change Healthcare. By reducing denials by an average of 40% within one year, providers can capture more revenue and significantly improve their bottom line.
Learn more about CLAIMS.AI
Schedule a demo today to see claim denial prediction and prevention in action.
Learn more